I found a pressure sensor matrix that we could adapt to a pressure sensor patch on the stomach of the women in labor on this webpage (see below). It gives instructions how to build a pressure sensor by using two pieces of cloth and conductive thread! If I understand it right, you just have to sew everything together in the explained way and connect it with external pull-up resistors! They even provide the Arduino code. Click through the pictures on the top, all steps are explained in detail and a video is provided in which you can see how it works.
http://www.instructables.com/id/Pressure-Sensor-Matrix/
We should try this! Maybe we can make it as a sticky patch… something that looks like this guy!
http://www.vni1.com/available/freedom-patch
What do you think?
Home Stretch
by Grace Yao
It’s crunch time now! MIT Museum 1-minute pitches this Saturday, and 15-minute presentations in class next week.
We’ve finally chosen a team name: Team Partayuda, from the Spanish words for “birth” and “help.” So here’s what’s up, as far as I know…
Maysun is working on the breadboard and programming for the pressure sensor – a capacitor, with rubber in the middle, and [AB] is going to make it. We tried making the EMG last week, but it did not work out.
Karina found the cool conductive thread project that she just posted, so she and [LT] are going to try to make that happen; [LT] is also working on Arduino code for the button.
So in total we should have 3 different ways of input to test (which may or may not happen before class presentations): the capacitor, the conductive thread, and the button…I think right now the button is the closest to being finished.
I’m going to work on the processing code to take the input and provide an output of the results we want to show. However, we don’t have the monitor yet, so this may end up just being displayed on a computer. [AB] and I are going to put together the poster, including the problem statement, our solution, Pugh chart, Design Compass, and design specs among other things, while [LT] is going to make a slide for the museum pitch.
Busy week, but we’re almost there!
Response From Nicaragua
by [LT]
Hi All,
Our contacts in Nicaragua have kindly responded to our questions with very interesting information that has really defined our problem. See their responses below.
- The women know about when to arrive at the hospital. They receive information when they receive their prenatal checkup. Births can happen during transport due to the distances involved. Women don’t have ready access to an OB/Gyn and subsequently need to travel up to 4 hours to receive specialized attention.
- The monitoring is crucial in knowing the condition of the mother and the fetus.
- We use a medical method in which we place a hand over the patient’s abdomen for 10 minutes and perceive the contractions. We have immense difficulties because of the large number of patients. There are only 2 doctors per shift for 15-25 patients which need to be monitored every 4 hours and apart from that, we need to attend to births and do cesareans and fill out a stressful amount of paperwork. On occasion, we don’t manage to monitor all the patients and are limited to just asking if they have had pains and with what frequency. To listen to the fetal heart rate, we use a stethoscope. Often, we don’t listen to it because we have to move them around to listen to it with a fixed ultrasound which takes up more time.
- To give you an idea of how difficult it is to monitor all the patients, before every shift, we pray to God that [the room] is not too full.
- To see if it would cause the mother stress, it would be necessary to conduct a study, and that depends on various factors, but for us it would be very valuable information.
- Don’t know if it will be effective or not. For that, we’d have to try it, but I think that for the level of education, it would be better that they didn’t participate (I think he means that due to their lack of education, they wouldn’t do it right- they shouldn’t have control of the input of the monitor).
- Contraction control is crucial. We do it every four hours when the expectant mother doesn’t have any labor problems and each hour when she is in labor. This last case we control the labor through the partogram.
Instructable
by Grace Yao
I think the Processing code this girl wrote could be helpful to us right now (although our pulse ox code might already do the trick for now); the entire Instructable might be useful in the long run for future work.
http://www.instructables.com/id/Fabric-bend-sensor/
“Using conductive thread, Velostat and neoprene, sew your own fabric bend sensor.
This bend sensor actually reacts (decreases in resistance) to pressure, not specifically to bend. But because it is sandwiched between two layers of neoprene (rather sturdy fabric), pressure is exerted while bending, thus allowing one to measure bend (angle) via pressure. Make sense? Watch below:”
By the way, our team name is now Babytrakr!
Pennies for Your Muscles
by Maysun M. Hasan
Hey,
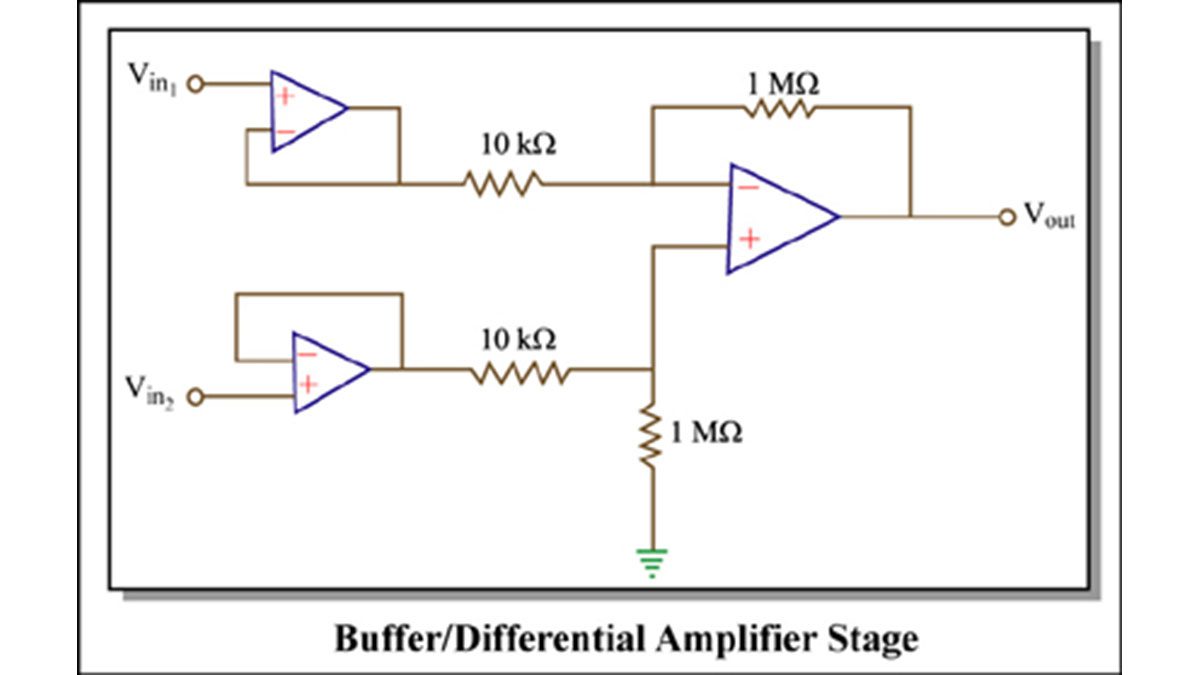
So I totally suck at blogging!!! I have a lot to say about the progress of our device that has happened in the last week. The last time I wrote, I had a plan for the EMG and I was about to build. Well I built it and realized that this was not the best way to do it… This is the schematics for it anyways.
Image by MIT OpenCourseWare. Adapted from circuit designed by Ankit Gordhandas, Irena Hwang, and Vinay Ramasesh.
This is the differential amplifier stage I described earlier. I built it, along with super cheap, super cool electrodes 🙂 (See below)
Pennies as electrodes
Yes… they are pennies that I soldered to wires… but they work so whatever. So I build the circuit with LM741’s (the most typical op amp you can get)…and… it didn’t work. I know it was able to take the difference between two signal… but not muscle signals. So I did some research and found out that because it is such a tiny signal… and better op amp is necessary. So I used LT1637’s for the buffer and a LM358 as my amplifier. And… it didn’t work. After debugging though… I found my signal… But!!! It was tiny and very noisy!!! Also it was not the same shape as we thought it would be. It marked when the muscle started to contract, but not the whole contraction. This signal was so inconsistent that I felt it would not be the best for our prototype. That is why EMG was out… but what now… we have no input… Well this is where the capacitor idea that is mentioned in a few of the blog entries comes in. Sorry for the weird timeline… I am horrible at posting.
Convo with Dr. Acker
by [AB]
Thanks Mays for reminding me to post also! Sorry this is very late and happened 2 weeks ago but here’s how the conversation with Dr. David Acker from Brigham and Women’s Hospital went:
1) What do you use to measure contraction?
- he measures the frequency, duration, and intensity of each contraction
There are 3 subjective ways to measure:
- ask woman how much it hurts and to record frequency of contractions on paper
- place monitor on abdomen and when contraction causes stomach to rise the pressure sensitive device will monitor by graphing on a slowly moving strip of paper (can’t record the intensity of the contraction with this device, however.)
- membrane ruptured and tubing placed through vagina into uterine cavity—intra-amniotic pressure measured and this is the most precise way to measure contractions but it’s invasive and uncommonly used
2) How does the tocodynamometer work?
- Measures contraction rise by pressure sensitive sensor (device is like a piston)
3) When do you know baby is coming?
- Contractions occur every 5 minutes lasting 1 minute each for the past hour, then the baby is going to come soon
- There is monitoring of the woman even a week before the baby comes
- Labor is not defined by the contraction rate, it is defined by the contractions leading to a cervical change (that’s where the partogram comes in)
- Rock hard cervix until contractions loosen it for opening
- Fetal heart rate response indicates complications (our device will notify the doctor when the contraction ends so he can check the fetal heart rate, it will not have a fetal heart rate monitor…yet?)
- On average, the fetal heart rate shouldn’t change, but when fetal heart rate increases → reassuring because indicates an acid/base balance
- When fetal heart rate decreases → various patterns so doctor needs to determine which pattern happens to see what is wrong
4) What smarts are the best out of EMG, flexiforce or push button?
- In the US, Dr. Acker doesn’t believe a push button will be effective because we’re simply replacing a pen and pencil for the women to a ball. However, he thinks it might help if they are in lots of pain and don’t wish to record their contractions.
- He thinks the rubber pressure sensor is a very cool idea, however, the abdominal muscle or rather skin on top of the abdomen doesn’t harden so the pressure sensor should be something that notes rises in abdomen (~1 cm rise, Maysun’s mom also said the same thing)
- Women’s abdomens are different so an external sensor needs to accommodate these variations
- Thickness of abdominal wall also varies
We took all these answers into consideration when brainstorming for our prototype two weeks ago. As you can see in the post below, our prototype changed numerous times because we wanted to accommodate all the ideas and comments from doctors in Nicaragua and the US. Ultimately, we went for a pressure sensor that is different from a toco, but still measures abdominal rise for contraction rate to correlate to a hand squeeze ball. Dr. Acker also agreed to let us see his operation room if we needed some more ideas, so if the project continues we have access to his resources. He was very nice about answering questions and very interested in helping out in the future. Here’s his profile:
http://physiciandirectory.brighamandwomens.org/directory/profile.asp?dbase=main&setsize=30&last_name=Acker&pict_id=0000063
For more detail: BabyTrackr